Healthcare Engineer
Engineering systems that close the structural gaps where healthcare access repeatedly fails as healthcare evolves faster than its design.
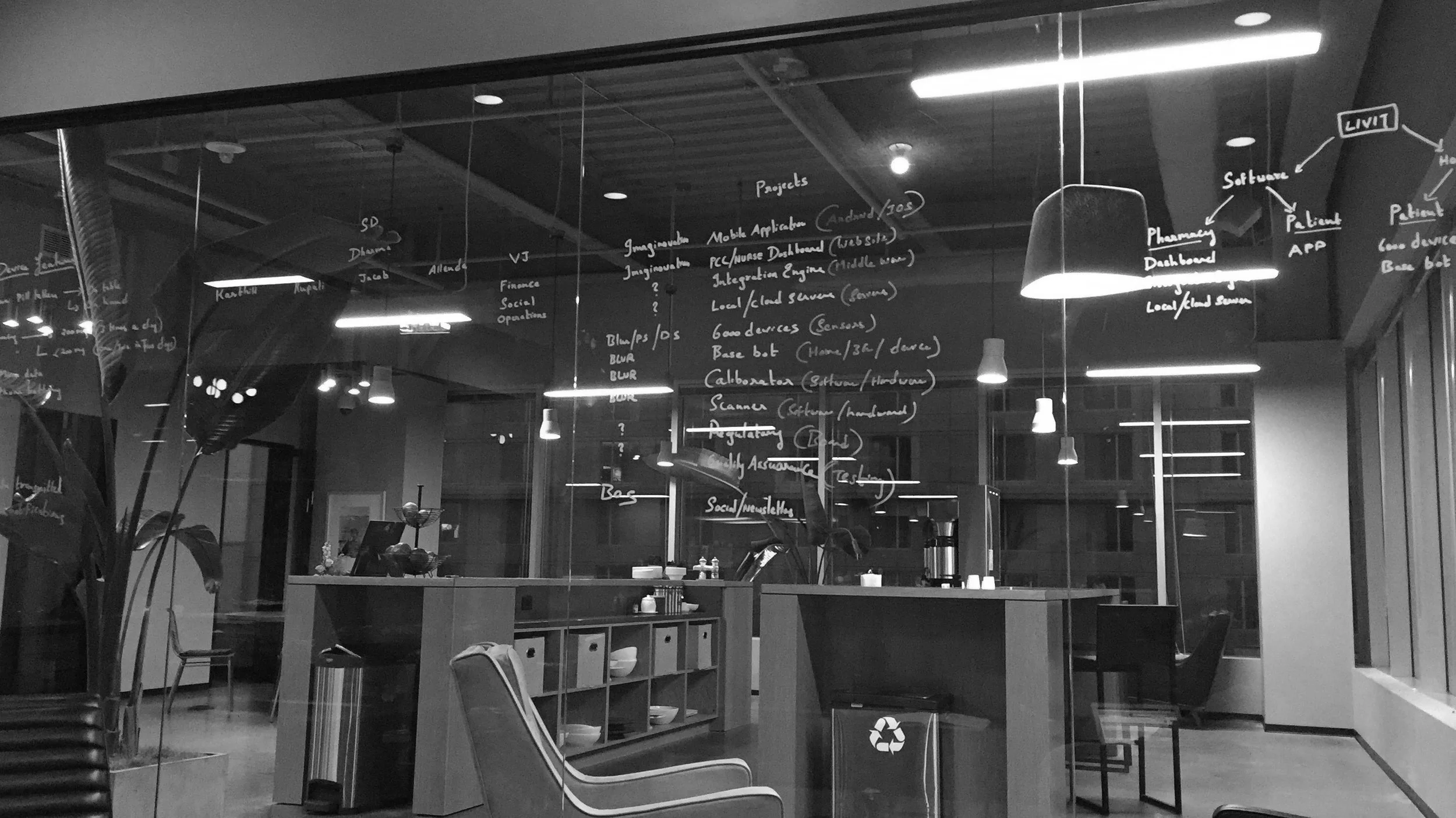
A systems-engineering approach shaped by real-world exploration across digital health, mobile care infrastructure, clinical operations, and assisted living environments.
Modern healthcare rarely fails because technology or infrastructure is missing. It fails because systems are not designed to adapt as care delivery models, cost structures, regulation, demographics, and patient needs evolve. As a result, access becomes inconsistent.
Patients often reach one part of the system—screening, diagnosis, consultation—only to lose access at the next step due to fragmented workflows, rising costs, institutional handoffs, or operational bottlenecks. Care exists, but continuity does not.
Healthcare access is therefore not a static problem. It is a systems problem, recreated continuously as the world changes faster than healthcare systems are redesigned.
Why Healthcare Access Fails ?
What a Healthcare Engineer Does ?
A Healthcare Engineer applies systems engineering to healthcare access.
The work focuses on identifying where and why access fails—physically, economically, operationally, or structurally—and then re-engineering end-to-end systems that make access consistent, reliable, and executable under real-world constraints.
Rather than optimizing isolated technologies or infrastructure, this approach designs structure, workflow, economics, and operations together, so that access does not collapse between screening, diagnosis, treatment, and pharmacy.
Why the Healthcare Engineer Path ?
The Healthcare Engineer approach emerged from an engineering background, not from healthcare ideology.
With formal training in computer science and networking engineering, early work focused on building technology solutions for large enterprises. These systems often addressed complex, high-value problems and functioned exactly as designed.
Over time, it became clear that even the most sophisticated organizations were constrained—not by lack of technology, but by structural gaps they had learned to operate around rather than resolve. These gaps persisted across workflows, cost structures, regulatory boundaries, and organizational incentives.
In healthcare, those gaps directly translate into loss of access for patients. As an engineer, the logical response was not to build more isolated technology, but to study the gaps themselves—understand why they exist, why they persist, and how systems must be redesigned to close them.
This led to the creation of multiple concepts and platforms, not as products in search of revenue, but as engineered responses to real access failures. Success and failure were measured less by short-term outcomes and more by whether each system reduced fragmentation and made healthcare access more consistent and reliable.
The Healthcare Engineer identity reflects this commitment: to pursue true healthcare problems and engineer solutions that work under real-world constraints, regardless of market cycles or individual outcomes.
An Access-Centered Systems Approach
Healthcare access breaks in different ways at different layers. Each concept developed under this framework addresses a specific class of access failure:
Access is treated as a system property, not a feature.
-
visibility, engagement, and continuity of information
-
care delivered where patients are
-
cost-aware models aligned with reimbursement
-
removal of institutional and workflow bottlenecks
-
stabilizing utilization through care-environment control
Core Concepts
Each concept operates independently, yet integrates into a larger access system.
LIVIT
A digital health framework focused on engagement, adherence, and real-time visibility into care behavior. LIVIT addresses access loss caused by information gaps, delayed response, and lack of continuity after clinical decisions.
IMASQ
An intelligent mobile healthcare access system designed to close physical and operational access gaps. IMASQ enables diagnostics, screening, treatment, and follow-on care to reach patients through purpose-built mobile infrastructure.
From Exploration to Execution
This work has progressed through multiple cycles of exploration, stress-testing, scaling, pausing, and redesign—across different markets and care settings. Each phase produced operational learning that informed the next.
From early digital health research to pandemic-scale mobile healthcare, and from mobile dental services to assisted living operations in the United States, the consistent objective has remained the same: make healthcare access reliable end-to-end.
Assisted living environments expose access failures clearly: residents often lose care due to transportation limits, staffing constraints, and fragmented service delivery.
By integrating mobile care delivery with assisted living operations, access can be stabilized rather than episodic. Ownership and operational control of care environments allow demand, utilization, and continuity to be engineered rather than assumed.
Assisted Living as a Control Layer
Who This Work Is For
Seniors and populations experiencing access fragmentation
Healthcare operators seeking scalable, real-world delivery models
Strategic partners aligned with systems-level innovation
Investors focused on durable platforms rather than point solutions
Explore Further
Vision & Philosophy
Platforms & Concepts
Mobile Healthcare Systems
Assisted Living Operations
Journey & Learnings